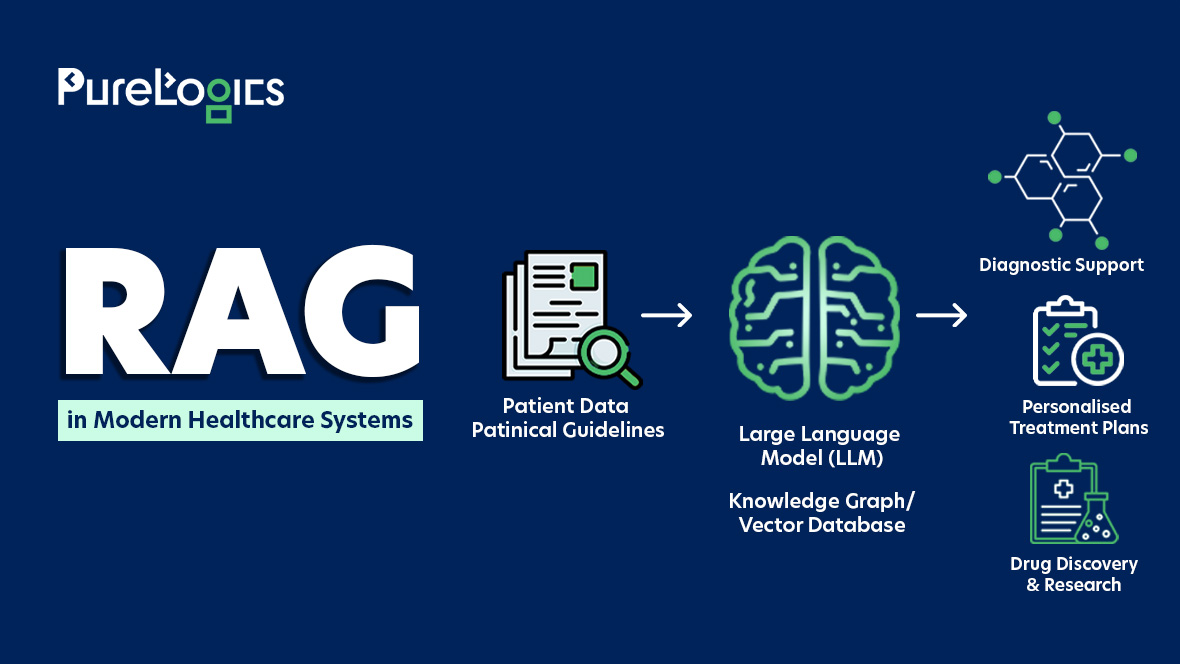
Large Language Models (LLMs) in healthcare are improving patient care, decreasing workload, and enhancing operational efficiency. Yet using LLMs in this domain is not without challenges, especially when it comes to strict data and patient privacy protection regulations. Researchers often fine-tune pre-trained models such as GPT, LLaMA, or PaLM with clinical data, but these models can become vulnerable to security threats and data breaches.
Furthermore, inconsistent data preprocessing across research teams can also increase the risk of exposing protected health information (PHI). To overcome these challenges, the healthcare institutions can build HIPAA-compliant LLMs that protect patient data.
This piece explores two strategic pathways: building versus adapting HIPAA-compliant LLMs, highlights critical practices for healthcare leaders in enabling LLM adoption, and concludes with what the future holds in this regard. Starting with the importance of HIPAA compliance in LLM.
Importance of HIPAA Compliance in LLM Adoption
HIPAA mandates the protection of patient health information (PHI) in the US. Any organization that gathers, stores, and processes PHI must comply with HIPAA regulations.
Moreover, Large Language Models (LLMs) deployed in clinical practices, whether for summarizing notes, answering patient queries, drafting care plans, or processing medical records, are exposed to PHI and therefore fall under HIPAA’s scope.
The stakes indeed are high:
- Healthcare remains the costliest industry for data breaches. (IBM)
- The healthcare breaches cost an average $398 per exposed record. (Veriti)
- Healthcare breach detection and containment time remains high, at roughly 279 days for healthcare in 2025. (HIPAA Journal)
These statistics show the gap between the complexity of healthcare data and its existing security frameworks. Moreover, the continuous rise in breach cost indicates that traditional compliance approaches are no longer helpful, and organizations must adopt HIPAA-compliant LLMs. That integrates intelligence directly into compliance operations, allowing:
- Continuous monitoring
- Rapid anomaly detection
- Automated PHI classification
All in all, deploying HIPAA-compliant LLMs requires a structured approach that balances innovation with data governance. From outlining clear use cases and classifying PHI to implementing secure deployment models and continuous validation, each step ensures safe and scalable adoption. Some of the recommended LLMs are LLaMa 3, Gemma, Dolphin, Phi 3, and Falcon LLM. Moreover, the organizations can move towards retrofitting or building one from the ground up.
Two Roads to HIPAA Compliant LLMs: Build vs Adapt
As healthcare AI matures, organizations face a pivotal decision regarding whether to enhance the existing LLM or build a new one from the ground up. Each path to HIPAA compliance requires precision, security, and strategic foresight, determining how deeply regulatory trust is embedded in the model’s design.
Retrofitting Compliance into Existing LLMs
Many healthcare organizations already use LLMs for administrative automation, clinical documentation, or patient engagement. Most of the models were not designed with HIPAA in mind. To make them compliant, the focus should shift to retrofitting privacy, access, and monitoring controls into existing pipelines. Below is the strategic way to make the already existing LLMs HIPAA-compliant.
Conduct a Comprehensive HIPAA Assessment
Assess data flows, access points, and model operations to identify vulnerabilities where PHI exposure or logging risks may occur across the AI lifecycle. Add a data lineage verification step to ensure no PHI remnants exist in model checkpoints, embeddings, or logs generated during pre-training or fine-tuning.
-
Strengthen Encryption and Access Control Layers
Apply enterprise-grade AES-256 encryption and enforce RBAC to safeguard data both at rest and in motion, ensuring only verified access to sensitive assets.
Automate PHI Redaction and Contextual Filtering
Integrate intelligent redaction engines and adaptive context filters to remove the inadvertent PHI exposure within the model outputs or logs.
-
Adopt Private, Compliant Deployment
Deploy LLM within HIPAA-eligible cloud infrastructure (AWS, Azure, or GCP) under the signed BAAs to ensure compliant data storage and processing.
Continuous Monitoring and Real-Time Compliance
Establish proactive monitoring to ensure consistency in HIPAA-compliant LLM with audit logs, anomaly detection, and an alerting mechanism to detect any deviations before they amplify into compliance breaches.
Architecting Compliance-First LLMs from the Ground Up
Building from scratch allows healthcare organizations to integrate compliance directly into the model’s design rather than as a policy afterthought. The Privacy by Design ensures regulatory integrity across the model lifecycle, providing security, scalability, and trust in the healthcare systems.
Data Sourcing & Preparation
Data integrity builds the foundation of a HIPAA-compliant LLM, and it is better to use only de-identified or synthetic PHI, eliminating all 18 HIPAA identifiers, such as names, SSNs, and addresses. Partner with a trusted healthcare software development company to help you gather data without exposing the PHI.
Secure Model Training Infrastructure
Compliance mandates a secure training environment, so it is better to train exclusively in AWS, Azure, or GCP with signed BAA, apply AES-256 encryption for stored data and TLS 1.2+ for data in motion, enforce RBAC and MFA, and routinely scan logs and checkpoints to avoid any data leakage. This helps ensure PHI confidentiality across model development.
Privacy Preserving Learning Techniques
Privacy-enhancing computation allows model training without sensitive data exposure. Furthermore, federated learning should be used to retain the data within institutional boundaries, whereas differential privacy can help prevent memorization of PHI in training gradients. Lastly, synthetic data augmentation can improve generalization while avoiding identifiers. These safeguards are essential in protecting regulatory and ethical compliance. Additionally, deploying secure multiparty computation (SMPC) and homomorphic encryption allows the model to process sensitive medical data without ever decrypting it directly during training or inference. These safeguards are essential for maintaining both regulatory compliance and ethical standards in healthcare AI.
Model Architecture and Storage
The architecture is responsible for the compliance resilience and isolating model weights and inference APIs in a Virtual Private Cloud (VPC), restricting all the external API that are outside the compliance perimeter, maintaining the immutable audit trails for every update, and conducting penetration testing and red team simulations to identify PHI leakage vulnerabilities. Additionally, integrating API gateways with automated PHI detection and request throttling helps secure against inadvertent data exposure during inference.
Evaluation & Compliance Validation
Shift compliance from periodic audits to continuous assurance and automate the pipeline to flag PHI-like outputs. Integrate continuous red teaming and adversarial testing pipelines to simulate data leakage and prompt injection scenarios, ensuring the model’s compliance resilience against evolving attack vendors. As for interpretability, use Explainable AI tools like SHAP or LIME, and conduct quarterly HIPAA audits with independent penetration testing to maintain certification readiness and operational transparency.
Deployment & Access Control
Deploy through private endpoints, enforce end-to-end encryption, maintain role-based access logging, and implement incident response protocols for any breaches or anomalies to increase patient trust and maintain institutional reputation.
Governance and Ethical Oversight
Document all workflows for audit transparency, secure BAAs with subcontractors and data partners, and offer ongoing workforce training in AI ethics, HIPAA policy, and responsible handling of PHI.
Strategic Tradeoff
| Approach | Speed | Long-Term | Compliance Depth | Ideal For |
|---|---|---|---|---|
| Retrofit (Existing LLM) | Fast | Moderate | Partial | Hospitals experimenting with Gen AI |
| Build from scratch | Slow | Low | Deep | Enterprises creating AI-based healthcare systems |
Whether retrofitting existing models or designing LLMs from the ground up, integrating HIPAA compliance is no longer optional. Healthcare leaders must adopt structured practices to ensure models fulfill the regulatory, ethical, and operational standards. This lays the foundation for establishing HIPAA-compliant LLMs via actionable strategies and critical governance measures.
Critical Practices for Healthcare Leaders in Establishing HIPAA Compliant LLMs
Establishing HIPAA-compliant LLMs is a crucial task for healthcare leaders. Below are the measures they can take:
Vendor Management
HIPAA-compliant AI for healthcare is the future, and the organizations that depend on third-party vendors for LLM should ensure that these vendors comply with HIPAA. Some of the best practices can be:
- Establish BAAs with vendors handling PHI and conduct their regular audits to ensure ongoing compliance.
- Perform detailed due diligence before choosing vendors to ensure they fulfill HIPAA compliance requirements.
Training and Awareness
One of the significant risk factors in data breaches is human error; therefore, continuous training awareness programs for staff can mitigate the risks. Some of the best practices are given below:
- Hold regular HIPAA and data security training for employees.
- Conduct phishing simulations to raise awareness about email security.
- Design and enforce clear policies regarding the use and protection of PHI.
Data Minimization
Collect and use only necessary PHI for LLM applications to reduce the risk of exposure, and the following are some of the best practices:
- Limit the scope of data gathered to what is required or necessary.
- Implement data retention policies to ensure that PHI is not kept longer than necessary.
Mitigation of Bias
LLMs can generate biased outputs, which can affect patient care and privacy, and some of the practices to avoid any bias are given below:
- Use diverse data sets to train LLMs.
- Develop and implement ethical guidelines for the use of LLMs.
- Regularly audit LLM outputs for bias and implement corrective measures.
Legal and Regulatory Compliance
Staying updated with legal and regulatory requirements is essential for HIPAA compliance, and some of the practices that can be followed in this regard are given below:
- Regularly consult legal counsel with expertise in HIPAA and AI to ensure compliance.
- Build comprehensive compliance programs and policies and ensure they are regularly updated.
Following these critical practices, healthcare organizations can confidently move from strategy to implementation. Stanford Medicine’s Information Technology Health Care’s Secure GPT initiative demonstrates how HIPAA-compliant LLMs can be deployed securely and at scale.
Case Study In Focus: Stanford Healthcare’s Secure GPT
They deployed Secure GPT to give clinicians and researchers HIPAA-compliant AI access. Below was the challenge they were facing:
Context & Challenge
Stanford clinicians, researchers, and in-house developers wanted to use LLMs for clinical documentation, research queries, and operational workflows. However, consumer-grade LLM tools raised HIPAA, privacy, and data retention issues, and there was no approved internal channel to run sensitive queries safely. The challenge was to provide the productivity benefits of LLMs whilst ensuring all interactions with PHI remained within auditable and HIPAA-aligned controls.
Solution
The department deployed Secure GPT, an infrastructure offering private API-enabled endpoints to LLMs deployed in Azure OpenAI Studio. Furthermore, the key elements of the solution are below:
- Only the users from Stanford Health Care and Stanford School of Medicine with institutional login credentials can access the platform.
- The deployment includes proprietary OpenAI models (GPT-4o mini, GPT-4o, GPT-4, GPT-4-32k, GPT-3.5-Turbo, text-embedding-ada-002, DALL-E 3) and open-weight models (TinyLlama, Llama-2), all accessible through private Azure endpoints.
- PHI never exits the controlled environment, and model interactions are isolated to prevent feedback into model weights or external retention.
- The system enforces Azure’s Confidential Computing environment (TEE-based) for runtime encryption, ensuring data is protected even during active computation.
Results/Benefits
- Secure LLM access: Clinicians and researchers can safely perform tasks such as clinical note summarization, literature synthesis, research queries, and image generation.
- Reduced compliance risk: Centralized deployment and strict governance minimize uncontrolled PHI exposure.
- Safe environment: Secure GPT facilities, NLP experiments, bias evaluation, and other AI-driven pilots that require sensitive data.
- Strategic HIPAA compliance: Security, transparency, and continuous compliance are integrated into LLM architecture rather than being an afterthought.
LLMs have completely revolutionized the way in which healthcare systems operate and can prove to be a great ROI.
Cost of LLM Development
The cost of LLM development can be from $1 million to $6 million, and the development timeline can be 6 months or above. However, cost and the development timeline can change depending on the project requirements.
Get a Custom Quote for Your HIPAA-Compliant LLM
Share your requirements, and we’ll give you an accurate cost estimate tailored to your project.
With the expansion of the diversity of medical data, the role of LLM in enabling more precise, personalized medical diagnoses and treatments will increase.
Future Outlook
The LLM market is expected to reach a total value of $82.1 billion by 2033. In healthcare, medical applications currently account for 21% of global LLM usage, with 49% of healthcare institutions using models for diagnostics and 42% for patient engagement ( Source: Industry Research). Moreover, the fine-tuned LLMs are allowing faster drug discovery, predictive analytics, and personalized treatments, portraying the growing role of LLMs in shaping the global healthcare market. However, the LLM market in healthcare is estimated to reach $21.15 billion by 2034 (Source: Industry Research). Therefore, healthcare executives must act now to implement secure and HIPAA-compliant LLMs. By doing so, they cannot only achieve operational efficiencies but also long-term resilience and sustainable competitive advantage.
Takeaway
Deploying LLMs responsibly in healthcare is not just a technical initiative; it is a strategic investment in trust and compliance. HIPAA-compliant LLMs in healthcare can help in leveraging AI’s potential while protecting patient data, optimizing workflows, and driving smarter decision-making. Moreover, by embracing a compliance-first approach, healthcare leaders can change the regulatory requirements into a competitive advantage. With partners like PureLogics, organizations can design, deploy, and scale secure LLM solutions that redefine efficiency, safety, and patient outcomes. Book a 30-minute free call with our experts to tell us your needs and let us suggest the best possible solution.
Frequently Asked Questions
Are LLMs HIPAA compliant?
Not by default. LLMs like ChatGPT or Claude are not HIPAA compliant, but compliance depends upon how they are deployed and secured. They can only be HIPAA compliant if used in a protected environment with a signed BAA, proper data encryption, and no exposure of patient information.
Is OpenAI HIPAA compliant?
No, OpenAI is not HIPAA compliant and the public versions of ChatGPT and OpenAI’s API are not designed and developed to handle Protected Health Information (PHI). Healthcare organizations can only use OpenAI models in a HIPAA-compliant way if they are deployed through HIPAA-eligible platforms such as Microsoft Azure OpenAI with a Business Associate Agreement (BAA) in place.
What are the potential risks associated with using LLMs in healthcare?
The usage of LLMs without HIPAA compliance can introduce significant risks, such as data breaches, fines of up to $2.1 million per violation, and loss of patient trust.


 [tta_listen_btn]
[tta_listen_btn]
 October 20 2025
October 20 2025