The healthcare industry is at a critical juncture. Patients demand access to their medical records, real-time engagement, and personalized experiences, while providers are navigating rapid technology adoption, evolving regulations, and cost pressures.
AI, interoperability, and predictive analytics are mandatory for operational efficiency and revenue optimization, and leaders who understand these shifts and act decisively will set their organizations apart in a market defined by agility and innovation.
Key Figures Healthcare Leaders Must Consider Amid Market Shifts
- 72% of patients want easy access to their medical records (World Metrics).
- 115.5 million patients will use RPM by 2027 (Strategic Marketing Research).
- 65% are happy to share their data if it enhances the quality of care (World Metrics).
- 90% of patients at risk of ventricular dysfunction were correctly detected by AI (Mayo Clinic).
- The healthcare compliance software market is projected to reach $6.80 billion in 2030 (Grand View Research).
Healthcare executives need to assess these market shifts, develop actionable strategies, and modernize their workflows by creating patient-centered digital experiences. The following ten tips highlight the areas that will determine which organizations stay ahead and which fall behind in 2026 and beyond.
10 Tips Healthcare Leaders Can’t Ignore [2026]
These ten tips highlight strategic actions that leaders must prioritize in 2026 to stay ahead.
1. Scale Generative AI and Agentic AI to Modernize Operations Across All Functions
Healthcare organizations that deploy AI across multiple functions, rather than isolating it within specific departments, can reduce administrative burdens and enhance consumer experiences. Leaders who operationalize AI in any form, whether generative AI or agentic AI, with transparent governance, measurable ROI, and secure integration into core systems, will gain sustained efficiency and resilience.
Those who delay will risk fragmented operations, rising costs, and competitive disadvantage. For instance, fragmented AI pilots increase compliance risks and operating costs, plus prevent organizations from realizing enterprise-wide ROI.
61% of the healthcare leaders say they intend to pursue partnerships with third-party vendors to develop generative AI solutions.
Action Plan: Map the critical workflows where generative or agentic AI can deliver measurable impact (claim processing, revenue cycle, clinical documentation, and patient engagement), avoiding the trap of siloed pilots. Next, deploy AI, keeping in mind compliance, secure data integration, and real-time performance dashboards to ensure ROI is tracked and risks are mitigated.
2. Establish Strategic Technology Partnerships with Clear ROI Frameworks
Building and maintaining advanced in-house digital solutions can be challenging due to talent shortages and high costs. That’s why the majority of healthcare leaders are seeking strategic technology partnerships, especially for developing advanced generative AI solutions. Additionally, collaborating with technology partners allows hospitals to access specialized expertise, implement AI and predictive analytics more quickly, and deliver patient-centered solutions without burdening internal teams.
70% of surveyed health care executives plan to pursue alliances with technology companies in 2026.
Source: Deloitte
Action Plan: First, carefully identify high-impact gaps through deep analysis of patient analytics, digital engagement trends, and operational workflows, because any misstep here can lead to missed opportunities. Identifying these areas that directly affect outcomes, operational efficiency, and revenue ensures technology investments deliver measurable results. Ignoring these insights can leave the organization vulnerable to rising costs, regulatory risks, and declining patient satisfaction.
Stop Guesswork and Build Smart Healthcare Solutions
Let our developers identify gaps, create a plan, and deliver custom solutions so inefficiencies, compliance risks, and missed opportunities don’t hold you back.
3. Prioritize Interoperability Across Systems to Ensure Timely Access to Patient Data
For coordinated care, the seamless data exchange between EHRs, lab systems, imaging platforms, and telehealth platforms is critical. Additionally, interoperability ensures clinicians have timely access to accurate patient information. However, hospitals that fail to adopt interoperable systems risk care delays, data errors, and redundancy.
The global healthcare interoperability solutions market is expected to reach USD 8.6 billion by 2030.
Source: Grand View Research
Action Plan: Start by assessing data silos and integration gaps across all clinical and operational systems. Additionally, implement standardized APIs and FHIR-based data exchange protocols to allow real-time interoperability.
4. Navigate the 340B Rebate Pilot as a Revenue Protection Strategy
The 340B rebate pilot model 2026 will restructure drug reimbursement for safety-net providers. Hospitals that proactively restructure 340B programs before the pilot expansion can gain a competitive advantage in Medicaid managed care negotiations; otherwise, they must bear high operational costs.
The operational cost of the rebate model can range from $50,000 to $150,000 per hospital, depending on claim volume and denial rates
Source: American Health Association
Action Plan: To effectively navigate the 2026 340B Rebate Pilot, start by using predictive analytics to stimulate pilot scenarios across revenue, drug procurement, and identify gaps that lead to losses. Then implement digital solutions that can automate rebate tracking, optimize claim validation, and ensure compliance with pilot requirements. Continuous performance monitoring through integrated dashboards helps hospitals adjust strategies in real time, turning the complex program into a competitive edge.
Cut 340B Pilot Costs and Risks
Confidently embrace the 340B Rebate Pilot model with custom solution development that automates rebate tracking and streamlines claims.
5. Design Digital Patient Experiences as Revenue and Retention Strategy
There is a growing emphasis on patient-centered care, and leaders must understand that patients today want more than just clinical treatment. They want timely access to services and personalized experiences, and failing to deliver patient-centered digital care puts hospitals at risk of lower satisfaction scores and declining revenue.
75% of healthcare consumers say they want personalized healthcare experiences, and 92% expect providers to send them customized reminders and messages.
Source: Zipdo
Action Plan: To provide exceptional patient care, leaders must openly embrace technology, such as telemedicine and patient portals, to improve the patient experience and integrate patient feedback to enhance services and care delivery continuously.
6. Develop Real-Time Data Infrastructure for Value-Based Care Performance
Data is an asset in healthcare, and embracing a data-driven approach is key to improved decision-making and delivering the highest-quality healthcare services. Additionally, it is critical not only for enhanced decision-making and increased operational efficiency but also for providing the highest quality of patient care. Hospitals that fail to invest in real-time data infrastructure risk delayed interventions, inefficient resource allocation, and missed opportunities. Thus, it falls behind competitors who leverage data to optimize outcomes.
59% of hospitals worldwide are deploying real‑time analytics systems as part of their data infrastructure.
Source: 360 Research Reports
Action Plan: Start by implementing electronic health records (EHRs) that provide real-time insights, use predictive analytics and AI-powered tools to optimize resources, and enhance patient outcomes.
7. Enhance Regulatory Compliance to Reduce Operational and Financial Risk
Healthcare is one of the most regulated industries in the world, and staying on top of an ever-changing regulatory landscape and complying with laws can be hard. HIPAA and other state-specific regulations will become stricter in 2026. For instance, HHS proposed HIPAA cybersecurity updates earlier this year, and the final rule is expected to be published sometime in 2026.
Key Proposed Changes in HIPAA Security Rules [2026]
- Perform vulnerability scans, annual audits, and penetration tests.
- Build data restoration procedures to recover critical data within 72 hours.
- Written documentation of all policies, procedures, plans, and analyses is required.
- Maintain an up-to-date inventory of technology assets and a map showing ePHI flow.
- Conduct detailed risk analyses identifying threats, vulnerabilities, and potential ePHI impacts.
- All implementation specifications are mandatory, removing the flexibility between addressable and required.
- Implement encryption, multifactor authentication for ePHI, and removal of unused software to reduce vulnerabilities.
Action Plan: Implement continuous risk assessments focusing on patient data, cyber threats, and third-party vendors, and turn the findings into actionable controls. Additionally, automation and standardized processes, including policy documentation, incident response plans, and compliance tracking, can help reduce errors and increase efficiency. Therefore, healthcare leaders must enforce data-centric security measures, such as encryption, multifactor authentication, and access controls, and validate them through regular audits and penetration tests.
8. Embrace Energy Efficient Solution
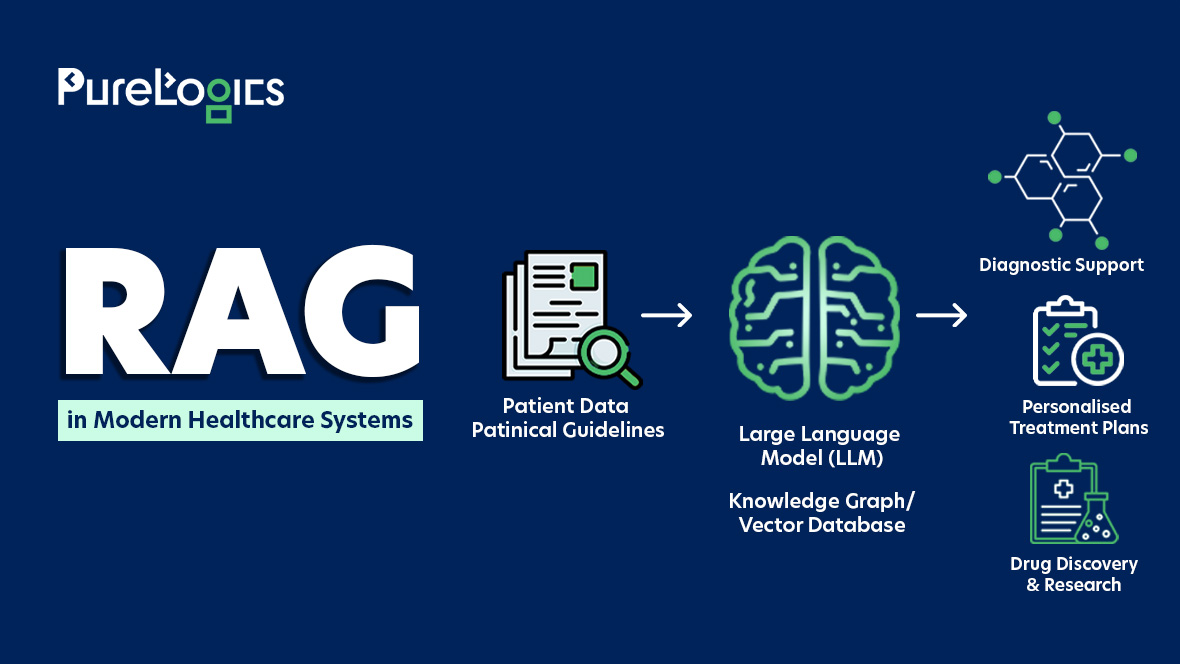
The use of AI in healthcare is increasing, with large language models (LLMs) supporting diagnostics, documentation, and patient care. However, the traditional AI systems are energy-intensive, creating costs and reliability challenges. Therefore, adopting healthcare technologies such as energy-efficient LLMs can help reduce energy consumption and prepare hospitals for growing data demands and rising energy costs, without compromising performance. Failing to adopt energy-efficient AI risks system outages, increase in operational costs, and falling behind competitors who manage both performance and sustainability effectively.
60% of hospitals globally have adopted some form of energy-efficiency program, indicating an increase in sustainability efforts in the health sector.
Source: Zipdo
Action Plan: Start by assessing current energy use and AI computing workloads to identify inefficiencies and adopt energy-efficient solutions to ensure system reliability. Then track performance continuously and integrate these measures into strategic planning and capital decisions.
9. Architect Zero-Trust Security Into Clinical Workflows
Hospitals and clinics rely on connected devices such as EHR systems, telehealth platforms, and AI tools, thereby expanding the number of potential entry points for cyberattacks. Thus, implementing zero-trust security with strict identity control and continuous monitoring is necessary. Any delay in adopting zero-trust risk management in 2026 can lead to data breaches, operational downtime, and regulatory penalties that could compromise patient care and organizational reputation.
The global healthcare zero‑trust security market will reach $22.12 billion by 2030.Source: Grand View Horizon
Source: Grand View Horizon
Action Plan: Enforce continuous identity verification for all users and devices accessing clinical systems, isolate high-risk applications and patient data, deploy real-time monitoring with automated threat response, and prioritize security of AI and telehealth workflows. Acting quickly on these measures reduces breach risk and ensures uninterrupted patient care.
10. Shift from Reactive to Predictive Care
Healthcare is traditionally reactive, responding to illnesses and complications after they arise. This approach often leads to more extended hospital stays and higher costs. In contrast, predictive analytics enables the anticipation of health events before they occur, enabling early intervention and reducing complications. However, in this era of AI, where patients expect personalized care, the hospitals that do not adopt predictive care risk higher readmission rates and increased operational costs.
The healthcare predictive analytics market size is projected to reach $67255.6 million by 2030.
Source: Grand View Horizon
Action Plan: Start by integrating real-time patient data from EHRs, wearables, and lab systems. Then deploy AI-driven predictive models to identify high-risk patients, implement proactive care plans, and continuously monitor results to refine models and enhance clinical impact.
2026 Healthcare Technology Readiness Assessment
Looking Forward
Healthcare leaders who act decisively will rule the future of patient care, operational efficiency, and revenue performance. Assessing technology, workflows, and regulatory readiness is no longer optional; it is essential for success. That’s why PureLogics helps healthcare organizations identify gaps, implement custom solutions, and optimize operations so they can deliver better outcomes while staying compliant and efficient. Our experts have over two decades of experience. Book your free 30-minute consultation with us.
Frequently Asked Questions
What will be the biggest challenge for healthcare leaders in 2026?
Balancing innovation with operational sustainability will be the biggest challenge for healthcare leaders in 2026. Moreover, to prepare effectively, healthcare leaders should start adopting technologies that deliver real results while ensuring patient data is protected, stay informed about changes in HIPAA, and make strategies to effectively embrace programs like the 340B Rebate Pilot to optimize cost management.
How will AI change healthcare operations and decision-making by 2026?
AI will make healthcare more efficient, helping healthcare staff make better decisions by handling routine tasks like scheduling and record-keeping, giving them more time with patients. It will also assist doctors in spotting health problems earlier and in suggesting treatments based on patient data on a larger scale.
Why will data security and compliance be more critical in healthcare by 2026?
In 2026, healthcare will be more dependent on digital records, devices, and online systems. This makes the protection of patient data mandatory, and any data breaches can harm patient trust. Moreover, healthcare organizations will face stricter rules and regulations, so ensuring strong security and compliance will be key to keeping patients safe.
How will patient experience influence healthcare success in 2026?
Patient experience will be a major factor in healthcare success, as patients now expect more personalized and easier access to care. Therefore, healthcare providers who focus on personalization will experience improved health outcomes and higher patient satisfaction.
How can healthcare leaders start preparing today for the changes coming in 2026?
Healthcare leaders should start preparing by focusing on a few key areas, such as staff training, improvement in digital experiences, adopting robust data security practices, and deploying AI on a small scale to assess what works.


 [tta_listen_btn]
[tta_listen_btn]
 December 29 2025
December 29 2025