Healthcare delivery has changed. Today, telemedicine software determines patient satisfaction scores, operational efficiency, and competitive edge. It also addresses the two critical needs of the healthcare industry: providing patients with faster, more convenient access to their providers, and reducing the administrative overhead for healthcare teams. This enables them to work more efficiently while expanding their capacity to serve a larger number of patients. In this blog, let us tell you more about the benefits of telemedicine software (from the patient and physician perspective), its types, key differences with telehealth software challenges you can face during development.
Bonus Section: In the end, we will reveal the core features that determine success rates and user engagement levels of telemedicine software.
First, let’s start with the problems a healthcare provider can face without telemedicine or telehealth solutions.
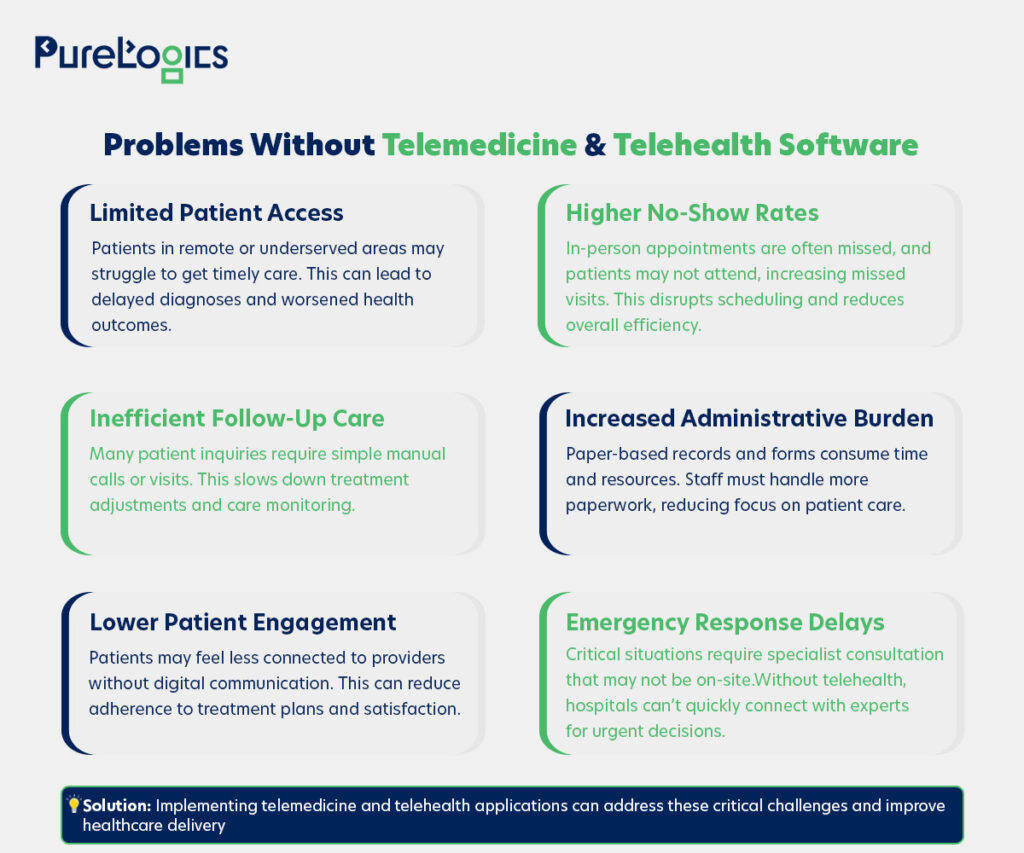
Challenges Hospitals Face Without Telemedicine & Telehealth Software
According to GoodRx Research, more than 80% of U.S. counties lack adequate access to healthcare services, and telehealth or telemedicine can prove beneficial in this situation. But healthcare organizations operating without modern virtual care capabilities can face several operational limitations, as shown in the image below:
Although people use telehealth and telemedicine terms interchangeably, they are different concepts. So, let us tell you all about it.
Telemedicine Software vs Telehealth Software: What’s the Real Difference?
Contrary to popular belief, telemedicine software development focuses on virtual clinical care, while telehealth encompasses broader digital health services. Below is an elaborate explanation to help you understand the concept further.
Telemedicine Software
It is the use of telecommunication technologies to facilitate the delivery of various medical, diagnostic, and treatment-related services, typically provided by doctors. For instance, it involves conducting diagnostic tests, tracking patient progress (after treatment or procedure), and supporting patient access to healthcare providers.
Telehealth Software
It is somewhat similar to telemedicine, but encompasses a broader range of remote healthcare services. Such as services provided by nurses, pharmacists, or social workers. For example, patient health education, social support, and medication adherence.
Now, let us tell you the difference between the two in a clear and concise form.
| Aspects | Telemedicine | Telehealth |
| Scope | Focused on remotely delivering clinical services | Covers both clinical and non-clinical services |
| Primary Use | Prescriptions, diagnosis, virtual consultations | Includes remote monitoring, patient education, and workflow tools |
| Users | Physicians, nurses, and patients | Physicians, patients, educators, and care teams |
| Goal | Improve access to remote medical care | Enhance overall healthcare delivery and management |
| Integration needs | EHR/EMR and billing systems | EHRs, hospital management systems, IoMT devices, and learning platforms |
| Examples | Video consultation apps and e-prescription systems | Telehealth platforms with portals, IoMT integrations, and analytics dashboards |
Due to its vast scope, the telemedicine and telehealth software market is experiencing significant growth and is expected to continue expanding in the coming years.
Telemedicine and Telehealth Software Market Overview
They both offer convenience and easy accessibility to healthcare services for patients, streamlining care delivery for practitioners, which is why they are on an upward trajectory.
- The global telemedicine market is expected to reach $451.4 billion by 2032 (Allied Market Research).
- As of 2024, there were over 116 million users of online doctor consultations worldwide (Statista).
- 99% of individuals who have used telehealth software were satisfied with it (National Telehealth Survey).
Besides making healthcare more accessible for patients and helping doctors keep track of their patients, it also integrates seamlessly with clinical workflows due to its different types.
Types of Telemedicine Software
There are two main types of telemedicine software, synchronous and asynchronous software.
Synchronous Telemedicine Software
It supports efficient information exchange and provides an opportunity to seek additional information and make clinical decisions in real-time. This is particularly helpful in urgent situations, as these solutions enable direct patient-provider communication and allow doctors to perform teleconsultations, telemonitoring, and other remote services.
Asynchronous Telemedicine Software
It allows the providers to send reminders and other messages without the need for live sessions. Thus, allowing practitioners to manage their schedules more effectively by designating time that works for them to review messages. This type is popular among specialties that require video or image sharing, such as dermatology, radiology, orthopedics, and ophthalmology.
The Future of Healthcare is Digital. Are You Ready?
Let us develop a HIPAA-compliant telemedicine app that scales with your practice and delivers super patient experiences.
Telemedicine and telehealth software help doctors engage with their patients at their convenience. Let us tell you more about the benefits from a patient perspective, too.
How Does Telemedicine Software Improve Patient Access and Provider Efficiency?
First, let’s discuss the benefits from the patient’s perspective, then we will move towards the doctors’ perspective.
Benefits of Telemedicine Software for Patients
- Convenience: This provides patients with access to high-quality care from their preferred location, eliminating the need for extended travel, waiting in queues, or scheduling in-person appointments. It is highly valuable for those living in remote areas with limited access to medical facilities.
- Accessibility: Telemedicine makes healthcare services available 24/7, from apps that monitor blood pressure to advanced and controlled surgical tools. The technology has empowered both the reach and quality of care.
- Reduced costs: Telehealth solutions, as well as telemedicine, have proved to be effective in reducing costs. It has enabled patients to access affordable packages, making healthcare more accessible to a broader audience.
- Continuity of care: Telemedicine solutions simplify follow-ups and send reminders for appointments, keeping patients on track with their care. This helps maintain consistent communication and prevents any lack in treatment.
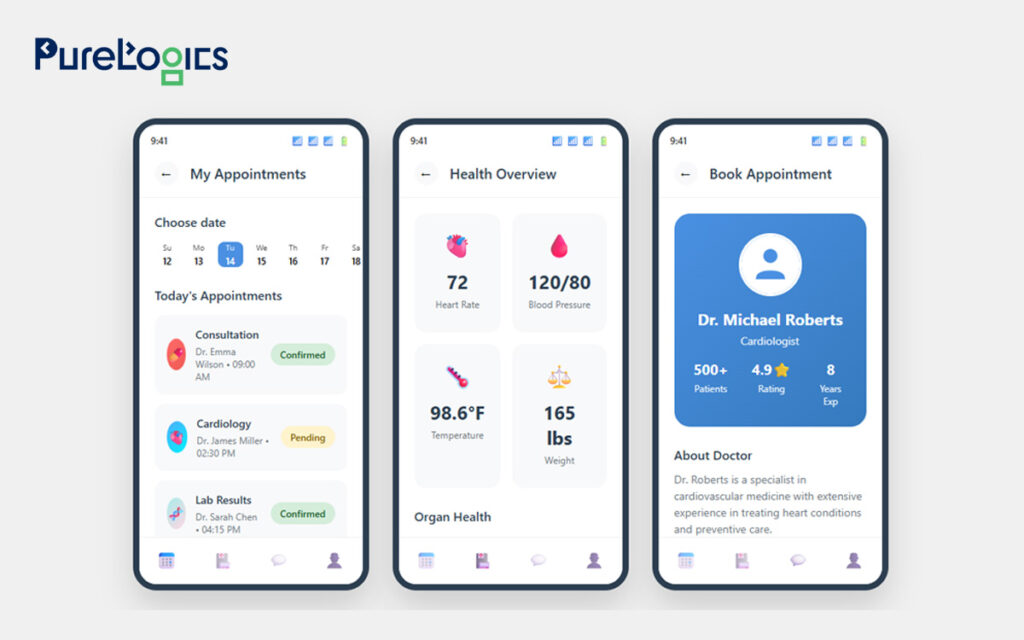
Below, in the image, you can see how a telemedicine app can help provide a full view and offer variations on booking appointments. Here’s the ideal interface of telemedicine software for patients.
Benefits for Doctors
- Decreased paperwork: Telemedicine apps decrease paperwork by digitizing patient records, forms, prescriptions, billing, and communications.
- Quick access to patient data: Some apps allow doctors to view basic patient history or notes, but the full EHR integration may require telehealth software.
- Follow-up care: These solutions help doctors monitor patient progress through video or messaging. Consequently, improving continuity of care and patient engagement.
- Reduced No-Shows: Virtual visits, facilitated by telemedicine, are more convenient for patients, resulting in fewer missed appointments. It also helps doctors manage their schedules more efficiently with fewer gaps.
- Efficient time management: The telemedicine apps effectively help physicians manage appointments, review patient histories, and adjust their schedules. This helps provide the work-life balance for doctors and saves them from burnout.
Below is the ideal interface of telemedicine apps for doctors.
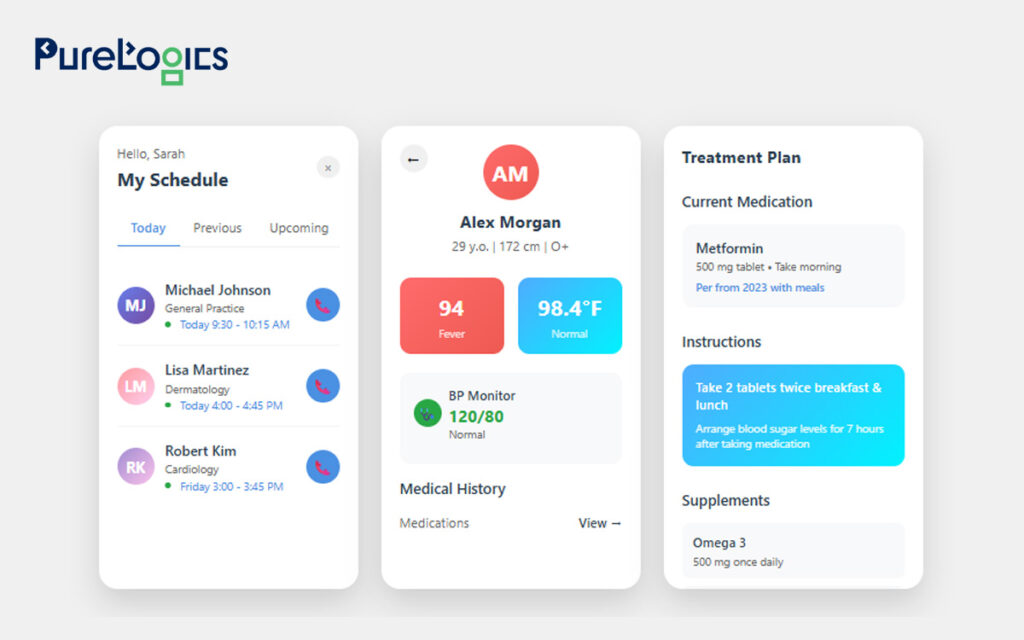
With these benefits, the telemedicine and telehealth software have completely revolutionized the healthcare industry. Indeed, they are now customary in enhancing patient health.
Ready to Transform Healthcare Delivery?
These interfaces aren’t just mockups; they can serve as your roadmap to delivering 24/7 care, reducing no-shows, and enhancing patient satisfaction.
Now it’s time for the bonus section we mentioned at the start, so if you are thinking about telemedicine or telehealth software development. Then, below are the key features you should include!
Essential Features for Telemedicine Software Development
The essential features that any telemedicine software should have are given below:
Easy Registration Process
The telemedicine apps should have an easy registration process. This means patients and doctors can register using their mobile numbers, email addresses, and third-party services, such as Facebook. Additionally, the registration process should meet EHR integration norms and allow easy document uploads for doctors.
Video Meeting
It is a key feature and should be of high quality to enable doctors to assess symptoms and determine diagnoses accurately. Moreover, video sessions must utilize HIPAA-compliant platforms with end-to-end encryption to protect PHI.
Text Messaging
This is one of the most essential features that enables patients to leave messages for their doctors, which doctors can read at their convenience. Additionally, you can also provide users with the option to attach photos or videos.
Appointment Management
It is a critical feature for both patients and doctors, enabling patients to track and manage appointments with doctors, while also helping doctors manage their schedules effectively.
Notifications
Besides calendar notifications, users can receive custom notifications to stay informed about prescription renewals, monthly visits, and physicians’ queries.
Payment Details
This feature is essential because integrating different payment options (PayPal, Stripe, and Braintree), among others, gives patients the flexibility to pay easily.
Dashboard
Dashboards in telehealth apps serve both doctors and patients by consolidating all information into one place. This can help doctors easily manage appointments, access patient information, and track follow-ups. Whilst patients can monitor their upcoming visits, prescriptions, and medical history.
Doctor Profile
It is an important feature that provides details such as doctor qualifications, specialization, experience, availability, and consultation fees. So, patients can make an informed decision and feel confident about the care they receive. For doctors, profiles can enhance professional visibility and facilitate more effective patient-doctor matching within the app.
Electronic Health Records
The telemedicine apps offer limited accessibility, whilst the telehealth software offers complete access to EHR and EMR. Moreover, EMRs provide a digital version of a patient’s chart within a single clinic, enabling doctors to track a patient’s medical history, diagnoses, and treatments. Additionally, EHRs allow the sharing of more detailed records across hospitals and specialists, ensuring continuity of care.
Whether it is a telehealth solution or telemedicine software, the development of both is challenging, primarily due to data security regulations that require the secure handling of sensitive data. If you think this is the only challenge, let us tell you about some other challenges you may face.
Challenges of Telemedicine Software Development
Developing a successful telemedicine solution presents challenges, particularly for hospitals and healthcare providers. Especially, with strict standards and increasing patient expectations. Below are some of the most common hurdles and how the right healthcare software development company can help you overcome them.
- Security: This is one of the biggest challenges, as healthcare data contains the most sensitive information, including personal identifiers such as email addresses, physical addresses, social security numbers, and credit card information. Additionally, healthcare experienced more cyber threats last year than any other critical infrastructure industry, according to the FBI’s Internet Crime Report. That’s why security measures like robust encryption, multi-factor authentication (MFA), role-based access control (RBAC), and strict session management are non-negotiable. Any breach can damage reputation and invite heavy penalties, making security-first development critical. Moreover, we ensure data protection with top certifications, including SOC 2, PCI DSS, and EPCS, demonstrating our commitment to protecting sensitive patient information.
- Regulatory compliance: Telemedicine software development must adhere to strict data protection regulations. Such as in the US, compliance with HIPAA is necessary (view this checklist to avoid HIPAA violations). In Europe, the GDPR and the EU Medical Device Regulation (MDR) are mandatory to follow. The globally recognized standards, such as HL7, FHIR, DICOM, and ICD-10, also play a key role. Without meeting these standards, the telehealth software risks legal complications, which can lead to limited adoption.
- Integration with existing systems: Hospitals highly rely on EHR/EMR platforms, e-prescriptions, Health Information Exchanges (HIEs), and remote patient monitoring tools. Therefore, it is essential to have a telemedicine app that integrates with existing healthcare systems. PureLogics specializes in HL7 and FHIR, ensuring that your telemedicine solutions seamlessly integrate into your existing ecosystem.
- Communication: There is nothing more frustrating for a doctor or patient than having an app that is slow to book appointments and send reminders. Therefore, it is essential to have an app that is highly dependable and serves both patients and doctors well. For instance, we have developed the platform CaringonDemand that connects patients with the nearest caretaker in their vicinity.
Indeed, the patient’s expectations are higher now more than ever, and real-time communication is a must. A strong telemedicine platform should minimize latency and deliver stable, high-quality video and audio for a professional consultation experience.
- User adoption & training: The best-designed software can fail if doctors, staff, or patients find it hard to use. Hospital ecosystems are complex and require a system that is easy to adopt and discourages the use of legacy systems.
- Scalability & maintenance: A hospital should have a platform that scales with its growth without any performance drops. Regular updates, feature enhancements, and compliance checks are crucial for maintaining system security and efficiency over time.
Conclusion
The MGMA (Medical Group Management Association) found that 73% of medical practices report patient no-show rates have stayed the same (60%) or decreased (13%) in 2025 relative to the previous year. Telemedicine and telehealth software can help reduce no-shows, enhance workflows, and ensure compliance. Indeed, these solutions address challenges that traditional systems cannot, but their development comes with hurdles such as data security, compliance, and interoperability, which a trusted healthcare software development company like PureLogics can effectively address. We combine our 20+ years of experience years of experience with deep industry knowledge and top certifications to deliver user-friendly telemedicine software.
Partner with us to confidently adopt digital healthcare and deliver better, more accessible care to your patients. Book your 30-minute free consultation with our experts!
Frequently Asked Questions
What are the steps for a nurse practitioner to start a telehealth practice?
To start a telemedicine practice as a nurse practitioner, you can choose a ready-made solution and set up workflows for scheduling, consultations, and patient records. But these solutions may not align well with your workflows, data structures, or compliance requirements. Plus, the licenses, add-ons, or workarounds can make them expensive over time. In contrast, you can hire specialist healthcare software developers to build custom solutions to get the features of your own choice. They are available for $15 to $ 20 per hour.
Will telehealth access end in 2025?
No, telehealth is not ending; however, some temporary COVID-era flexibilities, such as expanded coverage and relaxed rules, will expire on September 30, 2025, unless Congress extends them. It is better to build telehealth solutions that always stay compliant and adaptable to future regulations, as we do at PureLogics.
How do I start my telehealth practice?
Starting your own telehealth practice begins with identifying the care you want to provide and ensuring you meet all licensing and HIPAA compliance requirements. The next step is to set up a secure telehealth platform and integrate it with billing and patient management systems. With the proper setup, you can deliver convenient, efficient care while expanding your practice.


 [tta_listen_btn]
[tta_listen_btn]
 September 29 2025
September 29 2025